State Medicaid system transitions to managed care
By Andrew Dunn, Carolina Journal
After years of delays, North Carolina’s Medicaid program has finally transitioned to a managed care system — becoming the last large state to do so.
Starting July 1, the state's Medicaid system will be operated as a managed care program, essentially privatizing a system that once relied on the government paying medical providers directly based on how many procedures were performed.
Under the new system, the state will pay five health insurance companies $30 billion over the next five years to deliver health care to roughly 1.6 million people eligible for Medicaid in North Carolina. The system is designed to control costs, make budgeting easier and more accurate, and improve health outcomes by paying based on results instead of procedures and tests.
This Medicaid transformation, as it is called, has long had support from both Republicans and Democrats, though it was held up for years by Democrat Gov. Roy Cooper. His administration has now fully embraced it.
“We started this transformation to managed care to ensure North Carolinians get the quality, affordable health care they deserve,” Sen. Dan Blue, D-Wake, said in a statement earlier this year. “The transition to Medicaid Managed Care is far too important, and we intend to take all necessary actions to secure North Carolina's health care future."
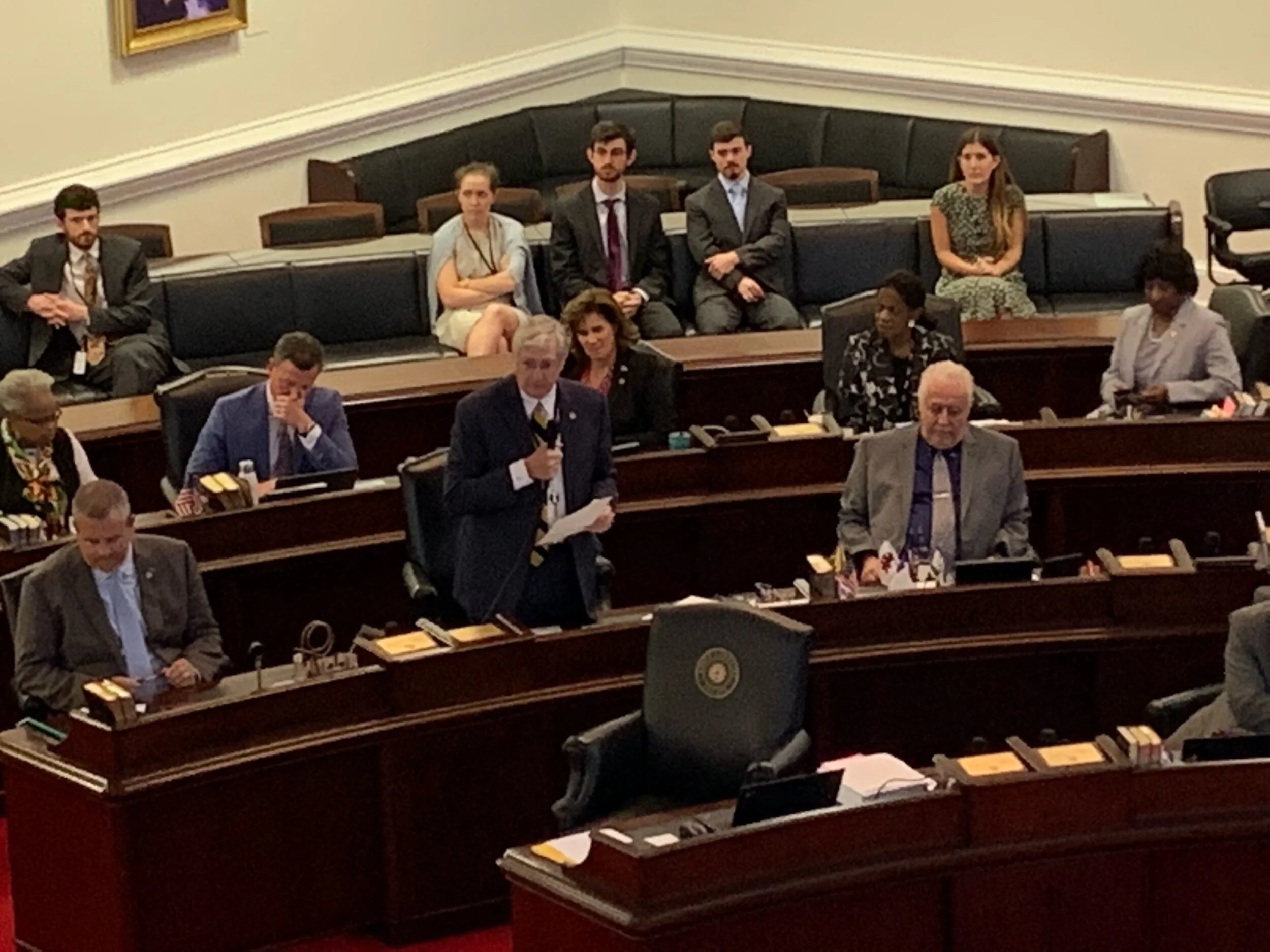
The move to managed care began in 2015, when the General Assembly passed a law directing the N.C. Department of Health and Human Services to move the state’s Medicaid system to a managed care program.
Under the old system, known as “fee-for-service” or “Medicaid direct,” DHHS paid doctors and hospitals directly for the health care services provided to people in the state’s Medicaid program. Medicaid covers low-income people who fall into one of a few categories: parents, people with disabilities, or elderly people. Costs have ballooned in recent years, overrunning budgets.
Most states — more than 40 — have already transitioned to managed care, and more than 75% of people in the U.S. receiving Medicaid are in one of these programs.
Under the system, the state pays managed care companies a fixed amount per month, per person enrolled. The companies are responsible for additional costs, but they also get to keep money saved. In North Carolina’s program, the state requires managed care companies to pay health care providers based on outcomes, not procedures.
Though the 2015 bill to start Medicaid transformation passed with significant majorities, Cooper attempted to stall its progress once he took office on Jan. 1, 2017.
The governor vetoed the budget in 2019, which provided money needed to complete the transition. He later vetoed a standalone bill that would have funded it. Under pressure, Cooper ultimately signed a 2020 bill to fund the Medicaid transformation process — though the rollout had to be delayed.
Part of the implementation involved getting Medicaid recipients to sign up for a managed care company plan and find a primary-care doctor. Open enrollment ran from March through May of this year.